How to book a covered treatment or request a reimbursement
Completing health care and expense claim forms
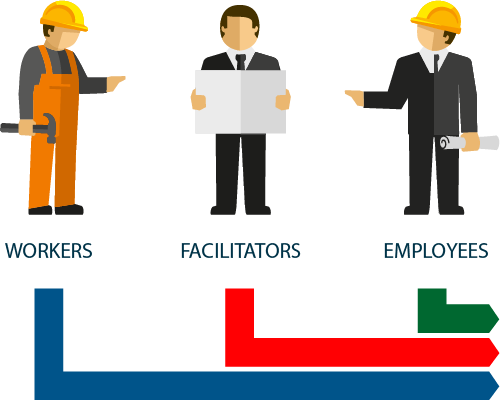
Registered company staff members
To apply for a direct medical benefit or reimbursement of medical expenses, it is always necessary to submit the form, which can be downloaded from this page, to the Cassa Edile/EdilCassa with which the worker is registered or, if he is not registered, to the Fund of the territory in which the company where the worker is employed is located, which must be completed and signed.
Family members who are the member’s tax dependants
To apply for a medical benefit or reimbursement of medical expenses attributable to the insurable member’s family (dependent spouse for tax purposes and family status and dependent children for tax purposes), it is necessary to submit one of the following forms to the Cassa Edile/EdilCassa with which the worker is registered/declared or, if not registered/declared, to the Health Insurance Fund of the territory in which the company where the worker is employed is based.
- If the insured person’s spouse/children are of age, the family member’s benefit/reimbursement request form must be completed and signed by the family member interested in the benefit, who may choose, indicating the details, to receive reimbursement of the expenses incurred on his/her own bank/post account, different from that of the insured person. The form also includes a section in which the family member can delegate the member to provide and receive information on claims and guarantees and to receive and deliver/send the relevant health documentation to the relevant Cassa Edile/Edilcassa.
- If the member’s children are minors, the application form for the benefit/reimbursement of minor children must be completed and signed by the insured worker who is the policyholder, who must also provide the bank details for crediting the relevant reimbursement of expenses incurred.
Applicants must attach to these forms the medical and administrative documentation required under point 2 below.
Please note: For the Fund to be able to correctly process a claim for a dependent family member for tax purposes, the certificate of the insurable family member, duly completed and signed by the employee, must first be submitted/sent to the Fund.
The certificate must only be resubmitted if there has been a change in the insurable family nucleus originally declared.
If the forms are not duly signed, even in the “Privacy Policy” section, it will not be possible to proceed with the processing of the request.
2
Documentation required for the correct processing of requests for health services and reimbursement of expenses
The following must be attached to the application forms referred to in point 1:

COPIA DELLA PRESCRIZIONE MEDICA/ IMPEGNATIVA
In the case of a request for a benefit under direct agreement:
- COPY OF THE MEDICAL PRESCRIPTION/REFERRAL with an indication of the pathology reported (certain or suspected) and of any diagnostic tests required
COPIA DELLA PRESCRIZIONE MEDICA/ IMPEGNATIVA
In the event of a claim for reimbursement of health care costs incurred, including from the SSN (National Health Service):
- COPY OF THE MEDICAL PRESCRIPTION/REFERRAL with an indication of the pathology reported (certain or suspected) and of any diagnostic tests required
- COPIES OF INVOICES/RECEIPTS FOR EXPENDITURE
- COPY OF AN IDENTITY DOCUMENT*
*This is only required in cases where the request is submitted by email.

COPIA DELLA PRESCRIZIONE MEDICA/ IMPEGNATIVA
In case of a claim for reimbursement for out-of-network implant services, please refer to the relevant page on the Fund’s website.
We recommend that you always keep a copy of the documentation submitted to the Cassa Edile/EdilCassa and the originals of the invoices/receipts.
Please note that failure to comply with any one of the above requirements will not allow the health benefit to be provided or the expenses incurred to be reimbursed.

3
How to submit claims for medical benefits and reimbursement
Claims for medical benefits and reimbursement can be made in the following ways:

Cassa Edile/Edilcassa Counter
Submission at the counter of the Cassa Edile/EdilCassa where the worker is registered or, if he/she is not registered, at the Cassa Edile/EdilCassa local to his/her place of work.
Before going to the counter, it is recommended to fill in the benefit request form (point 1) and bring the documents to be attached (point 2).
Designated person (facilitator)
The requirements of point A above may be provided through a facilitator (with the exclusion of services required for members’ family members).

Email or Registered Mail
Forward the documents referred to in points 1 and 2 to the Cassa Edile/EdilCassa with which the worker is registered, by email or by registered mail with return receipt; for the employee, refer to the Cassa Edile/EdilCassa of the province in which the company where he is employed is located.
Web Portal portale.fondosanedil.it
After registering in the Private Area of Fondo Sanedil’s web portal, members or their families can request a service from a network of approved partners or the reimbursement of a medical expense that will be taken over by the Cassa staff.
Learn the instructions.
4
AUTHORISATION PROCESS AND FULL BOOKING
AUTHORISATION PROCESS
Your Title Goes Here
The member/family member submits the benefit claim to the Cassa Edile/Edilcassa (point 3).
Your Title Goes Here
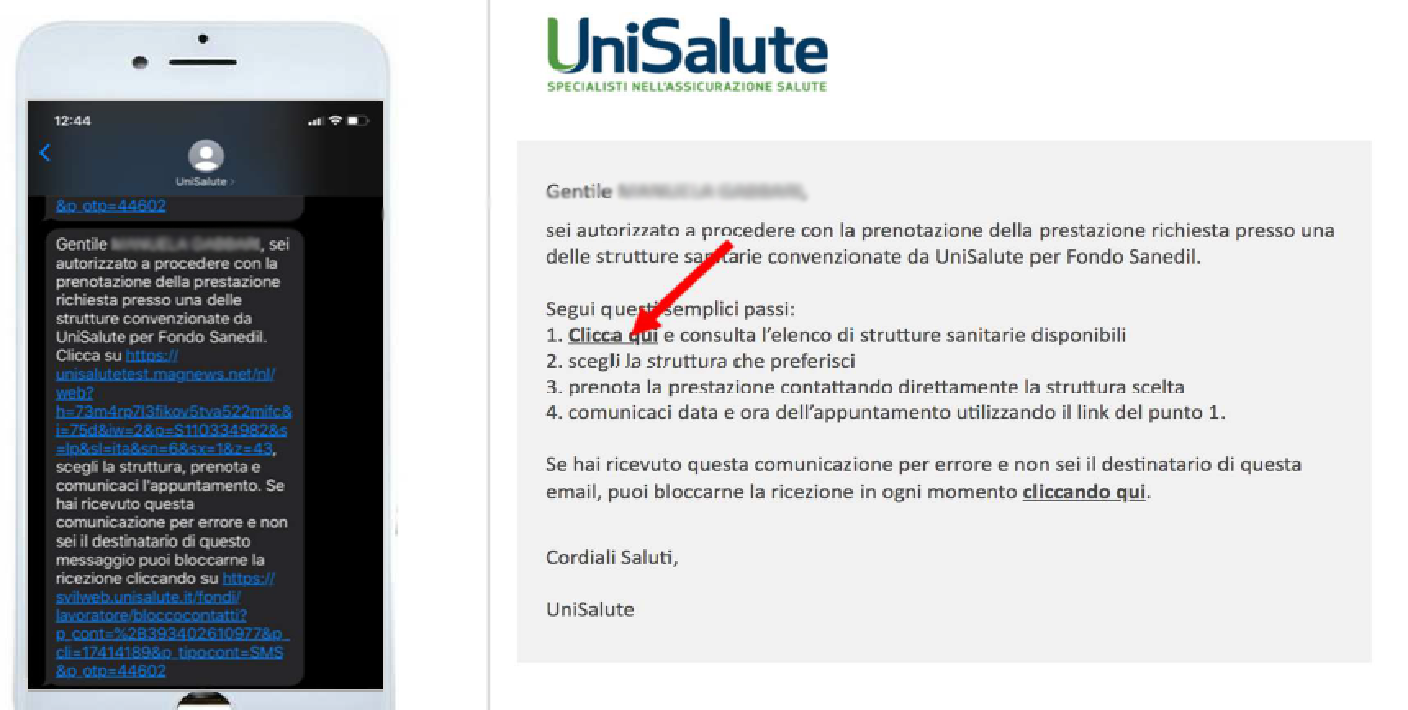
As soon as the Cassa staff have completed entering the data, the insured member/family member, if covered, will receive a text message and/or email confirming authorisation, with instructions on how to make the booking for the affiliated health facility themselves.
Your Title Goes Here
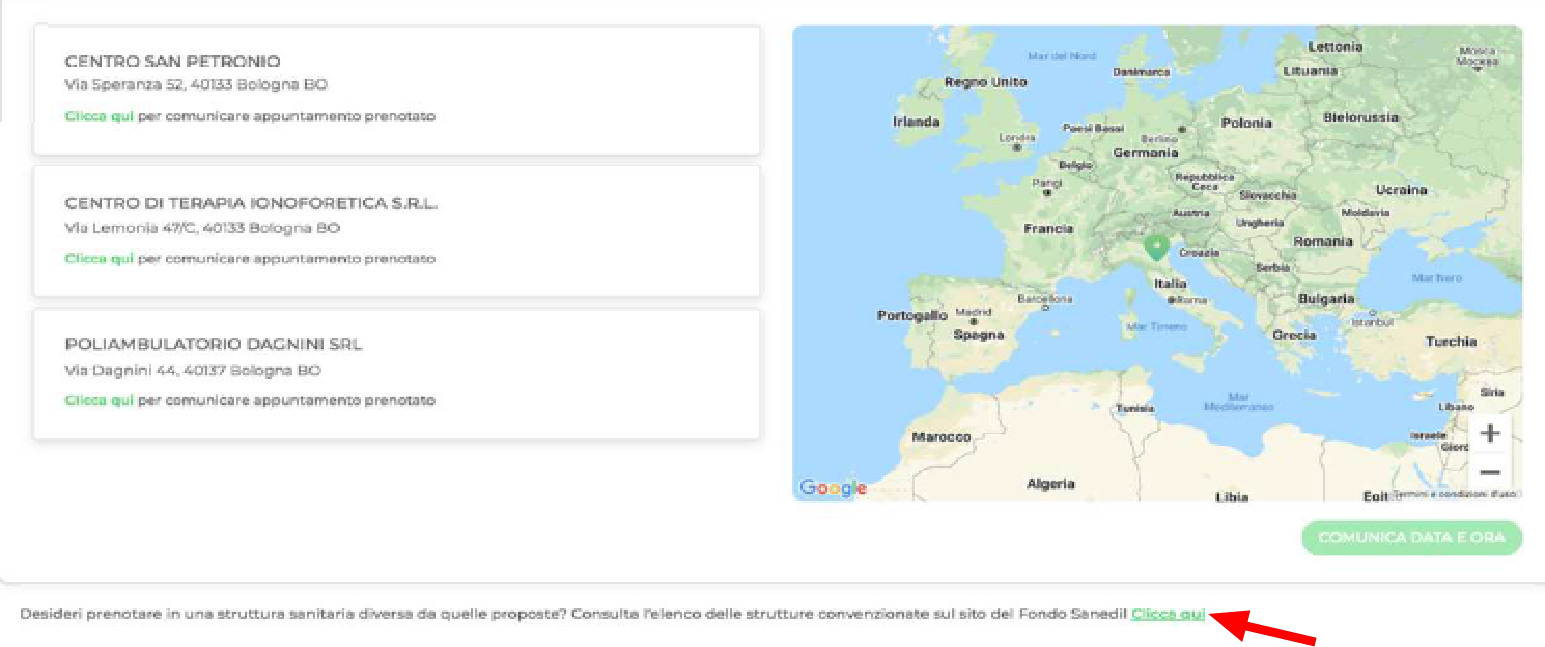
By clicking on the link in the email and/or text message, the subscriber/family member accesses the page for choosing the affiliated healthcare facility. The site offers a list of facilities to choose from.
Your Title Goes Here
By clicking on the chosen facility, the member/family member displays the facility’s contact details to make the appointment. He/she must also indicate the doctor with whom he/she will carry out the service.
When the member/family member contacts the healthcare facility, he/she must remember to indicate that he/she is insured with Fondo Sanedil – UniSalute.
Your Title Goes Here
If the member/family member wishes to choose a facility that has an agreement with the Fondo Sanedil other than the three automatically proposed by the system, he/she can consult the list of agreed facilities on the Fondo Sanedil website and then click on the appropriate link at the bottom of the page (see example below).
Your Title Goes Here
The member/family member should indicate the date and time of the appointment already agreed with the chosen health facility.
Your Title Goes Here
Once the member/family member has taken note of the summary of the appointment with the date and time entered, he/she will see all the information relating to the booking, including any fees he/she may have to pay. By clicking on “Confirm” he/she proceeds to send the information to UniSalute.
Your Title Goes Here
Once the booking procedure has been completed, the member/family member will receive a text message and/or email confirming the booking.
Please note that after receiving the booking authorisation text message, the member/family member has 15 days to make the booking at the affiliated facility, after which they will need to contact the Cassa Edile/Edilcassa to make a new authorisation request.
The associated facilities can be consulted here.
FULL BOOKING
The process differs depending on whether or not the member/family member has already made the appointment with the affiliated healthcare facility. In both cases, the procedure allows the member, who is unfamiliar with the application provided for the management of bookings with an authorisation process, to use the system offered by the funds to make a booking.
Please note that the healthcare facility must always be contacted personally by the member/family member to establish the terms of the appointment.
Full booking
WITH AN APPOINTMENT
The insured member/family member submits the request for benefits to the Cassa Edile/EdilCassa (punto 3).
If the member/family member has already made the booking with a facility that has an agreement with the Fund, he/she will hand over the required documents to the Cassa staff (points 1 and 2A), indicating on the request form the chosen health facility and the date and time of the appointment. In the case of specialist visits, the name of the doctor who will provide the service must also be indicated.
Upon completion of the booking procedure by the cashier, the member/family member receives a text message and/or email confirming the booking.
WITHOUT AN APPOINTMENT
The insured member/family member submits the request for benefits to the Cassa Edile/Edilcassa (point 3).
As the member/family member has not yet booked the affiliated structure/medical agreement, he/she hands over the required documentation to the Health Fund employee (points 1 and 2A), without any indication of the appointment time.
The member/family member then contacts the affiliated health facility in person, makes the appointment, and promptly communicates the terms of the appointment (health facility, date and time of the appointment, as well as the name of the doctor who will provide the service in the case of specialist visits) directly to the Cassa staff. Failure to do so will result in the reservation not being confirmed if the Cassa staff has not been informed of the terms of the appointment.
Once the booking procedure has been completed by the Cassa staff, the member/family member will receive a text message and/or email confirming the booking.
Points of attention in the health service/reimbursement request process
1
Claims for medical treatment or reimbursement can only be made for claims incurred from the effective date of the relevant healthcare plan.
2
The following are entitled to the PLUS Health Plan:
• members in the manual worker category who received the APE (Construction Staff Seniority) benefit by the end of September of the year in which each insurance year (1 October-30 September) begins;
• members in the office worker category when 24 months of contributions to the Fondo Sanedil can be verified.
3
The following are entitled to the BASIC Health Plan:
• manual and office worker members who have not met the requirements for access to the Plus plan.
4
For dental services that are covered only by the DENTAL TREATMENTS envisaged in the medical plans, the applicant should NOT attach any medical documentation, as the dentist will send the medical history form provided by the insurance company. In any case, the applicant must expressly indicate this type of request in the space reserved in the form mentioned in point 1.
5
In the case only of DENTAL PREVENTIVE cover, the member must indicate “tartar removal” on the form referred to in point 1 in the space reserved for the description of the service requested. ONLY in this case, for the cover to be acknowledged, the member does NOT have to wait for the dental practitioner to send the medical history form to the Insurance Company and may use the service upon receipt of the text message and/or e-mail confirming the appointment.
6
Dental services are only covered on a reimbursement basis if the member uses the National Health Service.
The purchase of lenses, orthopaedic and hearing aids and expenses incurred through the National Health Service are covered exclusively on a reimbursement basis, if provided for in health plans.
For all other covers, reimbursement is only permitted if the member is domiciled/resident in a province with no affiliated healthcare facilities.
7
The member is required to declare on the appropriate form the existence of any other policies covering the same insured risk. If the same risks are covered by two or more insurances, even if they are related to the Fondo Sanedil (UniSalute and Unipol-Sai), they will be managed, in compliance with the contractual reimbursement limits, by both companies.
An insured worker who has already been reimbursed by another company for the same insured risk shall be paid only the amount remaining for which he/she is responsible, in accordance with the deductibles and maximums and net of the amount already reimbursed, which must be documented and certified.
8
The member is entitled to an additional period of insurance cover following loss of employment, for 60 days in the case of the Basic health plan or 90 days in the case of the Plus health plan. These periods are counted from the termination of employment on a monthly basis and not for individual days.
How to claim an accident

Reporting and opening an accident claim
The manual or office worker must submit the accident report form to the relevant Cassa Edile/EdilCassa in person or via a facilitator, or by email/registered mail.
Points to note in the reporting process
1
Applications may only be made for claims occurring after 1 October 2020.
2
It is very important that the form is filled in correctly and completely and signed by the applicant.
The following must be attached to the form:
- Available MEDICAL DOCUMENTATION as identified in the Accident Coverage Guide;
3
Claims must be reported within 24 months of their occurrence.
4
The member is obliged to submit any additional documentation on claims that have already been opened to the Cassa Edile/EdilCassa staff.
5
Solely for neuromotor rehabilitation services to be provided in research hospitals, and hospitals of national importance highly specialised in neuromotor rehabilitation, in accordance with Law no. 833/78 Art. 42 and subsequent amendments and additions, the member must apply exclusively to the facilities indicated here.
6
The member is required to declare on the appropriate form the existence of any other policies covering the same insured risk. If the same risks are covered by two or more insurances, even if they are related to the Fondo Sanedil (UniSalute and UnipolSai), they will be managed, in compliance with the contractual reimbursement limits, by both companies.
An insured worker who has already been reimbursed by another company for the same insured risk shall be paid only the amount remaining for which he/she is responsible, in accordance with the deductibles and maximums and net of the amount already reimbursed, which must be documented and certified.
7
The member is entitled to an additional period of insurance cover following loss of employment, for 60 days in the case of the Basic health plan or 90 days in the case of the Plus health plan. These periods are counted from the termination of employment on a monthly basis and not for individual days.

Informations and contacts
The member may contact the relevant Cassa Edile/EdilCassa to obtain information on the status of the reported claim.
On completion of the investigation, the Company shall pay the amount due directly into the member’s current account by bank transfer.